Description
Semaglutide (GLP-1) Peptide
Semaglutide (GLP-1) and glucagon-like peptide-1 are short peptides. The hormone is only 31 amino acids in length, and researchers suggest their primary physiological function is to lower blood sugar levels by increasing endogenous insulin secretion. It appears to protect beta-cell insulin stores by promoting the transcription of insulin genes and is associated with neurotrophic impact in the central nervous system and the brain. Studies in the GI system have observed that Semaglutide may significantly reduce appetite by slowing gastric emptying and bowel motility. Preliminary studies have also suggested the potential impacts of Semaglutide on the heart, fat and muscle cells, bones, liver, lungs, and kidneys.
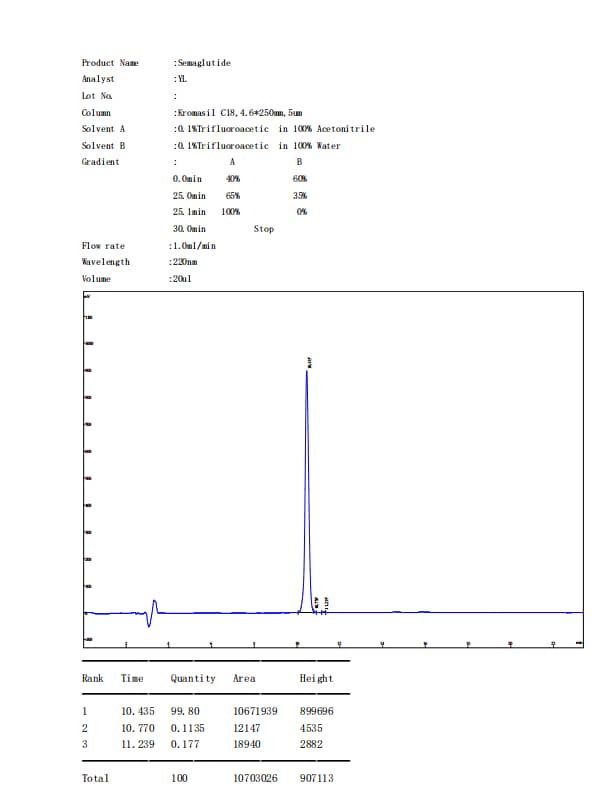
Specifications
OTHER KNOWN TITLES: GLP-1, proglucagon (72-108), glucagon-like peptide-1
MOLECULAR FORMULA: C187H291N45O59
MOLECULAR WEIGHT: 4113.64 g/mol
SEQUENCE: HXEGTFTSDV SSYLEGQAAK EFIAWLVRGR G
Semaglutide Research
SEMAGLUTIDE AND THE INCRETIN EFFECT
According to Holst, the most widespread association with Semaglutide is the “incretin effect.”[1] Incretins are a group of metabolic hormones released from the gastrointestinal tract that are considered to lower blood sugar levels. Semaglutide appears to be one of the two most common and essential hormones that may stimulate incretin action in the rodent model, alongside GIP. GIP appears to circulate at roughly 10x the concentration of Semaglutide, but there is data to suggest that GLP-1 may be more efficacious than GIP, particularly in cases of elevated blood glucose levels.[2] The researchers also note that “Decreased secretion of GLP-1 may contribute to the development of obesity, and exaggerated secretion may be responsible for postprandial reactive hypoglycemia.” Semaglutide receptors have been identified on the surface of pancreatic beta cells, suggesting that Semaglutide may directly stimulate insulin exocytosis from the pancreas. In combination with the sulfonylurea substance, Semaglutide has been suggested to increase insulin secretion.
Various potential impacts of the peptide include a possible increase in protein synthesis, decreased proteolysis, and increase in amino acid uptake by skeletal muscle. It is hypothesized that the peptide may interact with the GLP-1 receptors in the pancreas, potentially stimulating insulin production in pancreatic beta cells and possibly suppressing glucagon production by pancreatic alpha cells. According to the research teams exploring these hypotheses, the impact of Semaglutide appears to act in a glucose-dependent manner. Furthermore, it is suggested that the peptide may possibly aid in reducing the postprandial glucose spike following caloric intake. Studies have posited that it appears to slow gastric emptying, potentially by up to 38%, within the initial hours following calorie consumption.
SEMAGLUTIDE AND BETA CELL PROTECTION
Studies in animal models suggest that Semaglutide may stimulate the growth and proliferation of pancreatic beta cells and the differentiation of new forms of beta cells, precursors of pancreatic duct epithelium. Studies further theorize that Semaglutide may inhibit beta-cell apoptosis. These impacts may have the potential to upset the average balance between beta-cell growth and cell death. In terms of development, these research results posit the peptide’s potential within the context of diabetes research and indicate the possibility of the compound to protect the pancreas from attacks that damage beta cells. A compelling study indicated that Semaglutide appears to inhibit beta-cell death caused by elevated levels of inflammatory cytokines. In the mouse models of type 1 diabetes, it was observed that Semaglutide appeared to protects islet cells from destruction.[3] The scientists suggested that “It is possible that combined [exposure] could become a new strategy to defeat T1DM.”
SEMAGLUTIDE AND CALORIC INTAKE
A study of mouse models suggests that exposure to Semaglutide in the brain of mice may reduce the driving device and may inhibit caloric intake.[4] Semaglutide seems to induce satiation, reducing hunger hormone signaling in the brain. Recent trials have posited that GLP-1 receptor agonist may cause gradual weight loss in the case of murine models. This weight loss may lead to a significant improvement in cardiovascular risk factors and a decrease in hemoglobin A1C levels. Data from studies implies a potential link between the activation of GLP-1 receptors in the central nervous system, specifically in reward-related brain areas, and the modulation of appetite through GLP-1 receptor agonists.[5] In more specific terms, it is hypothesized that GLP-1 receptor agonists may interact with neurons located in the arcuate nucleus of the hypothalamus. These particular neurons appear to play a role in regulating appetite and hunger and are posited to express proopiomelanocortin and cocaine- and amphetamine-regulated transcript (POMC/CART). It is suggested that the potential activation of POMC/CART neurons by Semaglutide, a GLP-1 receptor agonist, may induce satiety while indirectly inhibiting the release of neuropeptide Y (NPY) and agouti-related peptide (AgRP), which appear to promote hunger hormone signaling.
Furthermore, studies propose that GLP-1 receptor agonists, such as Semaglutide, may assist in mitigating the decrease in free leptin and potentially elevate levels of peptide YY (PYY) 3-36 during weight reduction.[6] In a specific study, it has been suggested that Semaglutide appears to mediate a potential 35% reduction in mean energy intake during ad libitum eating, as compared to placebo (1736kJ vs. 2676kJ).[7]
SEMAGLUTIDE AND THE CARDIOVASCULAR SYSTEM
Semaglutide receptors are considered to be distributed throughout the heart, and may potentially improve cardiac function by increasing heart rate and lowering left ventricular end-diastolic pressure when present en masse.[8] A rise in end-diastolic pressure is often associated with left ventricular hypertrophy, cardiac remodeling, and ultimate heart failure. Recent studies suggest that Semaglutide may reduce the overall damage caused by a heart attack. The peptide appears to improve glucose uptake into the heart muscle; this may assist the struggling ischemic myocardium to maintain function and obtain the nutrients needed to avoid programmed cell death. Increased glucose uptake in these cells appears to be independent of insulin. High concentrations of Semaglutide in dogs have exhibited apparent improved and reduced LV performance and systemic vascular resistance. The latter impact may lower blood pressure. This process, in turn, may help reduce the long-term consequences such as LV remodeling, vascular thickening, and heart failure. According to Dr. Horst, introduction of GLP-1 after heart injury consistently appeared to improve myocardial performance in experimental animal models.
SEMAGLUTIDE AND THE BRAIN
There is data to suggest that Semaglutide may exhibit supportive activity in cognitive function and may potentially protect neurons from neurodegenerative diseases. One study has posited that Semaglutide may enhance associative and spatial learning in mice and improve learning in mice with specific gene defects. In rats that overexpress Semaglutide receptors in particular brain areas, both learning and memory were observed by researchers to be reportedly significantly better than controls.[9] Further research studies of mice indicated the peptide’s potential to protect from immunotoxic neurons. Interestingly, Semaglutide and its analog exendin-4 have been reported in mouse models to reduce amyloid-beta levels in the brain. The beta-amyloid precursor protein found in neurons is the primary component of the plaques observed in neurodegenerative disease.[10] It remains to be seen if preventing amyloid-beta accumulation might protect against the onset of Alzheimer’s disease. Still, this research is, at the very least, a tantalizing clue as to how scientists may further understand the progression of mild cognitive impairment to whole Alzheimer’s disease.[11]
SEMAGLUTIDE AND CAMP SIGNALING AT THE GLP-1 RECEPTORS
GLP-1 receptors are G-protein-coupled receptors (GPCRs) that are considered to be located on the surface of various cells, including pancreatic beta cells, brain neurons, and cells in the gastrointestinal tract. Semaglutide has been suggested to bind with GLP-1 receptors, where it may trigger a cascade of intracellular events. It is hypothesized that Semaglutide may bind to the receptor’s extracellular domain, potentially leading to a conformational change in the receptor structure. This conformational change may allow the receptor to couple with and possibly activate G-proteins inside the cell. It appears that Semaglutide may facilitate the binding of the G-protein to the intracellular domain of the receptor, which may potentially lead to the exchange of GDP (guanosine diphosphate) for GTP (guanosine triphosphate) on the G-protein.[12] The activation of the G-protein may subsequently trigger a signaling pathway involving the enzyme adenylyl cyclase. It is possible that the G-protein activates adenylyl cyclase, resulting in the conversion of ATP (adenosine triphosphate) to cyclic AMP (cAMP). Increased cAMP levels then may also lead to the activation of protein kinase A (PKA). PKA, in turn, may phosphorylate various intracellular proteins, including transcription factors and ion channels.
This phosphorylation cascade may potentially result in numerous downstream impacts as explored above. Additionally, researchers have posited that Semaglutide may activate the GLP-1 receptor-mediated phosphoinositide 3-kinase (PI3K) pathway. This pathway is considered to involve the activation of PI3K by the G-protein, potentially leading to the production of phosphatidylinositol 3,4,5-trisphosphate (PIP3). PIP3 may then activate downstream signaling molecules, such as protein kinase B (Akt). Hypothetically, Akt regulates various cellular processes, including glucose uptake, glycogen synthesis, and cell survival.[13]
SEMAGLUTIDE AND BETA-ARRESTIN SIGNALING AT GLP-1 RECEPTORS
Studies suggest Semaglutide may also potentially recruit beta-arrestins at the GLP-1 receptor, and it is hypothesized that beta-arrestins play a role in regulating GPCR signaling and internalization. If Semaglutide binds to the GLP-1 receptor, it may promote the recruitment and binding of beta-arrestins to the receptor. This recruitment may potentially lead to the desensitization and internalization of the receptor. Desensitization refers to the dampening of the receptor’s responsiveness to continuous stimulation, and it may occur through a process called receptor phosphorylation, where beta-arrestins might facilitate the addition of phosphate groups to specific sites on the receptor. Researchers posit that following desensitization, the internalization of the GLP-1 receptor may occur. This process is considered to involve the sequestration of the receptor into clathrin-coated pits, which then may form clathrin-coated vesicles. The internalized vesicles may transport the receptor to intracellular compartments for degradation or recycling back to the cell surface. The recruitment of beta-arrestins and the subsequent internalization of the GLP-1 receptor may contribute to the termination of signaling and enable the receptor to be available for future activation.[14]
It is worth noting that the recruitment of beta-arrestins at the GLP-1 receptor may also potentially initiate alternative signaling pathways independent of G-proteins. These beta-arrestin-mediated signaling pathways may elicit distinct cellular responses, including mitogen-activated protein kinase (MAPK) activation, which hypothetically regulates cell growth, differentiation, and survival.
Disclaimer: The products mentioned are not intended for human or animal consumption. Research chemicals are intended solely for laboratory experimentation and/or in-vitro testing. Bodily introduction of any sort is strictly prohibited by law. All purchases are limited to licensed researchers and/or qualified professionals. All information shared in this article is for educational purposes only.
References
- Holst JJ. From the Incretin Concept and the Discovery of GLP-1 to Today’s Diabetes Therapy. Front Endocrinol (Lausanne). 2019 Apr 26;10:260. doi: 10.3389/fendo.2019.00260. PMID: 31080438; PMCID: PMC6497767.
- Holst JJ. The physiology of glucagon-like peptide 1. Physiol Rev. 2007 Oct;87(4):1409-39. doi: 10.1152/physrev.00034.2006. PMID: 17928588.
- Yang Z, Chen M, Carter JD, Nunemaker CS, Garmey JC, Kimble SD, Nadler JL. Combined treatment with lisofylline and exendin-4 reverses autoimmune diabetes. Biochem Biophys Res Commun. 2006 Jun 9;344(3):1017-22. doi: 10.1016/j.bbrc.2006.03.177. Epub 2006 Apr 5. PMID: 16643856.
- Tang-Christensen M, Larsen PJ, Thulesen J, Rømer J, Vrang N. The proglucagon-derived peptide, glucagon-like peptide-2, is a neurotransmitter involved in the regulation of food intake. Nat Med. 2000 Jul;6(7):802-7. doi: 10.1038/77535. PMID: 10888930.
- van Bloemendaal, L., IJzerman, R. G., Ten Kulve, J. S., Barkhof, F., Konrad, R. J., Drent, M. L., Veltman, D. J., & Diamant, M. (2014). GLP-1 receptor activation modulates appetite- and reward-related brain areas in humans. Diabetes, 63(12), 4186–4196. https://doi.org/10.2337/db14-0849
- Ard, J., Fitch, A., Fruh, S., & Herman, L. (2021). Weight Loss and Maintenance Related to the Mechanism of Action of Glucagon-Like Peptide 1 Receptor Agonists. Advances in therapy, 38(6), 2821–2839. https://doi.org/10.1007/s12325-021-01710-0
- Friedrichsen, M., Breitschaft, A., Tadayon, S., Wizert, A., & Skovgaard, D. (2021). The effect of semaglutide 2.4 mg once weekly on energy intake, appetite, control of eating, and gastric emptying in adults with obesity. Diabetes, obesity & metabolism, 23(3), 754–762. https://doi.org/10.1111/dom.14280
- Gros R, You X, Baggio LL, Kabir MG, Sadi AM, Mungrue IN, Parker TG, Huang Q, Drucker DJ, Husain M. Cardiac function in mice lacking the glucagon-like peptide-1 receptor. Endocrinology. 2003 Jun;144(6):2242-52. doi: 10.1210/en.2003-0007. PMID: 12746281.
- During MJ, Cao L, Zuzga DS, Francis JS, Fitzsimons HL, Jiao X, Bland RJ, Klugmann M, Banks WA, Drucker DJ, Haile CN. Glucagon-like peptide-1 receptor is involved in learning and neuroprotection. Nat Med. 2003 Sep;9(9):1173-9. doi: 10.1038/nm919. Epub 2003 Aug 17. PMID: 12925848.
- Perry T, Haughey NJ, Mattson MP, Egan JM, Greig NH. Protection and reversal of excitotoxic neuronal damage by glucagon-like peptide-1 and exendin-4. J Pharmacol Exp Ther. 2002 Sep;302(3):881-8. doi: 10.1124/jpet.102.037481. PMID: 12183643.
- Perry TA, Greig NH. A new Alzheimer’s disease interventive strategy: GLP-1. Curr Drug Targets. 2004 Aug;5(6):565-71. doi: 10.2174/1389450043345245. PMID: 15270203.
- Graaf, C.d, Donnelly, D., Wootten, D., Lau, J., Sexton, P. M., Miller, L. J., Ahn, J. M., Liao, J., Fletcher, M. M., Yang, D., Brown, A. J., Zhou, C., Deng, J., & Wang, M. W. (2016). Glucagon-Like Peptide-1 and Its Class B G Protein-Coupled Receptors: A Long March to Therapeutic Successes. Pharmacological reviews, 68(4), 954–1013. https://doi.org/10.1124/pr.115.011395
- Shao, S., Nie, M., Chen, C., Chen, X., Zhang, M., Yuan, G., Yu, X., & Yang, Y. (2014). Protective action of liraglutide in beta cells under lipotoxic stress via PI3K/Akt/FoxO1 pathway. Journal of cellular biochemistry, 115(6), 1166–1175. https://doi.org/10.1002/jcb.24763
- Hager, M. V., Johnson, L. M., Wootten, D., Sexton, P. M., & Gellman, S. H. (2016). β-Arrestin-Biased Agonists of the GLP-1 Receptor from β-Amino Acid Residue Incorporation into GLP-1 Analogues. Journal of the American Chemical Society, 138(45), 14970–14979. https://doi.org/10.1021/jacs.6b08323

Reviews
There are no reviews yet.